When Dr. Catherine Hwang was diagnosed with breast cancer, a lot of her patients had the same reaction: “How can you have breast cancer? You’re a breast cancer doctor.”
“People think it’s not going to happen to them, so I really want to stress it is non-discriminatory,” says Hwang, a radiation oncologist at the AdventHealth Cancer Institute in Altamonte Springs near Orlando. “I’ve seen 20-year-olds with breast cancer, and I’ve seen 100-year-olds with breast cancer. If you have breasts, you can possibly get breast cancer.”
At age 46, she was tempted to put off her routine annual mammogram last year. She had a demanding medical practice, she had no family history of the disease and no symptoms, and she had three sons in travel baseball. She was planning a retirement party for a senior colleague. She was busy. But her best friend, breast cancer surgeon Devina McCray, convinced her to make time to get the mammogram done. “I said, ‘I’m going to walk you down there,’” recalls McCray, who recommends that women get an annual mammogram beginning at age 40, or earlier if they’re at higher risk.
During her mammogram, Hwang was told the news that no one wants to hear: “We see something.” After a biopsy was done, a few white spots on the scan turned out to be at least five tumors. Hwang hadn’t felt anything — anything at all. The diagnosis came as a complete surprise.
“The biggest tumor was actually over three centimeters. And a lot of people said, ‘How did you not feel that?’ And I said, ‘I didn’t.’ And this is why we do mammograms. I thought it would be just another Wednesday. It’s funny how the diagnosis stops the world.”
Next, an MRI showed cancer scattered throughout her right breast. As things proceeded, the news got worse and worse. Hwang ended up being shocked at how extensive the cancer was.
At the AdventHealth Cancer Institute where she works, a multidisciplinary care team took on her case. They’re designed to be a one-stop shop for cancer care. For Hwang, at first they recommended a mastectomy and endocrine therapy. She chose to have both breasts removed with reconstruction, and surgery uncovered more cancer. “Once they took me to surgery, five tumors ended up being more than 10.”
“She got it all — chemotherapy, radiation and anti-hormone pills. She got the kitchen sink.” —Dr. Devina McCray, breast cancer surgeon, AdventHealth Cancer Institute, Altamonte Springs
She was told she needed chemotherapy. And Hwang is a radiation oncologist, so when she looked at her own pathology report, she could see that she needed radiation too.
“She got it all — chemotherapy, radiation and anti-hormone pills. She got the kitchen sink,” recalls McCray, the breast cancer surgeon. “She’s experienced a majority of all the side effects you can get, so she really is able to sympathize with patients. Patients have taken to her for advice, because they know that she’s been through it.”
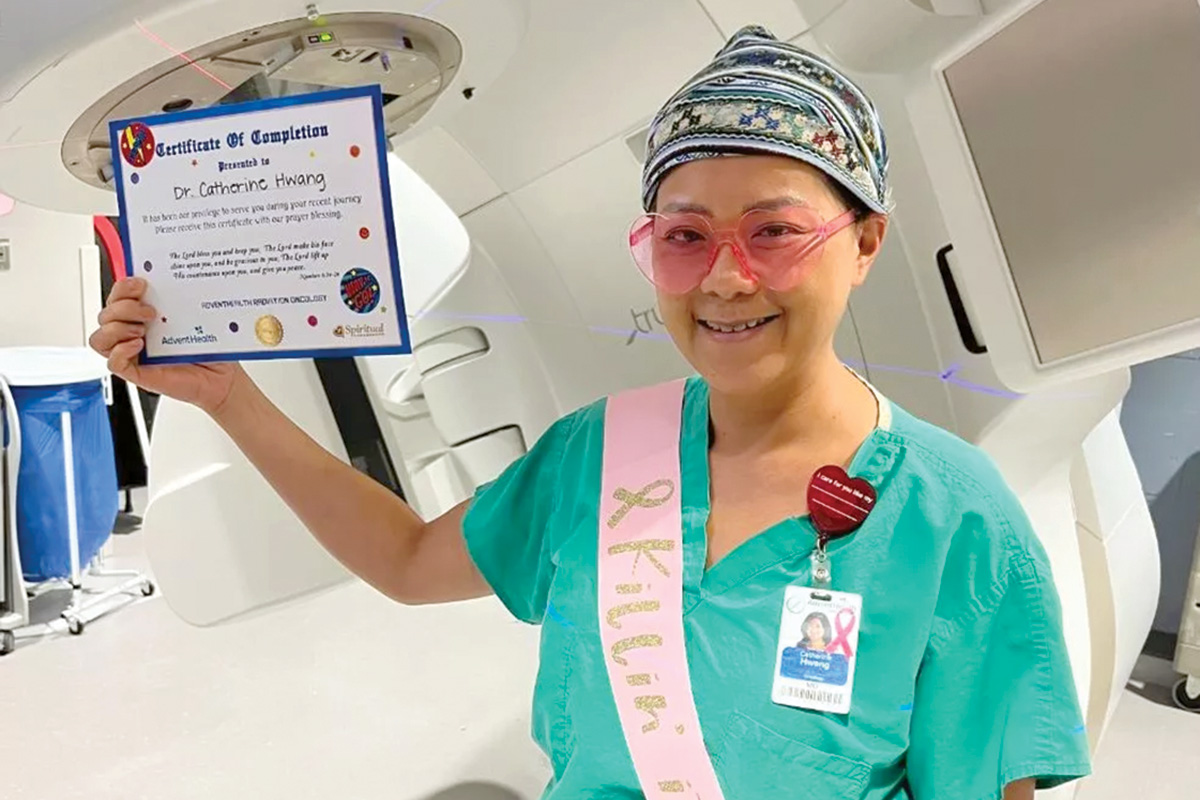
Hwang would see a patient, then get her radiation treatment, then go back to work and see another patient. She lost most of her hair. She got used to feeling fatigued. “These side effects — the fatigue — can be really debilitating and really quality-of-life altering,” she says.
Now cancer-free, what Hwang has taken from the experience has given her a deeper understanding of what her patients are going through — both during and after cancer treatment.
“When you finish treatment, you’re supposed to go ring this bell. And I was like, ‘Well, that’s great, I can ring the bell because it’s the end of treatment, but it’s not really the end of anything.’ Because I just kept thinking, ‘What now?’ Your treatment’s done, but it doesn’t mean that your fear of recurrence and fear of having cancer come back is any less.”
Cliche as it may sound, the experience has given her a deeper appreciation for her life. She feels that it’s made her a better doctor, a better friend, a better mother.
“For me, the biggest eye-opener is this whole world of survivorship, meaning life after cancer,” she says. “What I learned the most is that survivorship is a huge area of cancer care that needs more attention, and as doctors, we have to be more comprehensive and manage the patients on the back end just as well as we manage them on the front end.”
Cheaper Screenings
Beginning Jan. 1, screening for breast cancer will be more affordable for Florida’s state employees. A new law makes it so.
Right now, employees covered by the state’s health plan don’t have to pay for mammograms. However, they have to pay if they need any additional imaging like an MRI or an ultrasound.
If a mammogram shows something abnormal, the patient may need imaging to rule out breast cancer or confirm the need for a biopsy. An estimated 12-16% of women who get mammograms require imaging.
The out-of-pocket costs can be particularly burdensome on women who have previously been diagnosed with breast cancer, because diagnostic tests are recommended every time rather than just a mammogram. That’s according to Senate Bill 158, which was sponsored by the Senate Minority Leader, Sen. Lori Berman (D-Boynton Beach).

The new law expands state employees’ health coverage to include diagnostic breast imaging such as MRIs and ultrasounds. This is expected to cost $3.6 million a year, but legislators decided it was worth it.
“As a survivor of breast cancer, making sure more people had access to the treatment and testing that I did was very important to me,” Berman says.