When it comes to healthcare and insurance, every business is a consumer - searching for affordable, effective solutions to complex problems. In this special section, Florida's insurance and healthcare executives share their wisdom on how to access the data, analyze the options and make business sense of the risk of doing business today.
Nowhere is the bottom line impact of healthcare and insurance illustrated more clearly than in workers' compensation, where the dollars paid out by businesses can far exceed the cost of the insurance premium. The National Safety Council estimates workplace accidents cost $116 billion annually, with only one-third of that covered by workers' comp insurance. The rest is the hidden cost of replacing and retraining employees, and management time.
The way for companies to reduce these costs, says Robert J. Brautigam, senior vice president and division manager in Tampa for Liberty Mutual Insurance Co., is through loss prevention, not premium minimization. Gary J. Wynn, division manager of business sales, adds that companies that shop strictly on price are shortsighted about the costs they're incurring.
Liberty Mutual is a Fortune 500 company with worldwide presence in commercial insurance, personal lines and life insurance, and other financial services, and has been a leading writer of workers' comp coverage in Florida since 1925. With 25 local loss prevention professionals applying the findings of Liberty Mutual's Research Center for Safety and Health, the company takes a consultative approach to its mission of "helping people live safer, more secure lives.
"We involve the customer, from the employee up," Brautigam explains. The goal is to identify workplace conditions that cause accidents, and to show management a dollars-and-cents reason to make changes.
Brautigam says not every insured focuses on the fact that when workers return to light duty, lost days are reduced and the indemnity portion of the premium is impacted positively. "We look for ways to instill that thinking," he says, "and we work to convince the medical community that employers can offer an environment where early return is safe and a good thing for everyone."
Comprehensive Approach Delivers Benefits
Edward Peddie, president and CEO of AvMed Health Plan, a not-for-profit managed care plan active in 33 Florida counties, finds a quality problem in American healthcare. "Despite all our investment," he explains, "people are still dying unnecessarily because delivery is disjointed."
Peddie says managed care's comprehensive approach has enormous impact on healthcare quality. Disease management programs reduce both the cost and the incidence of lethal and crippling diseases through early detection and active assistance in managing symptoms and making lifestyle changes that limit hospitalizations.
AvMed is working on technological assistance to help overcome "the disjoint" in healthcare. Plan members will soon have Internet access to background and surveys on participating physicians, along with maps to their offices. And AvMed doctors will be able to use a private web that consolidates members' health records from all doctors involved in their treatment.
Peddie is excited about the potential of this "clinical repository" to improve and streamline healthcare. "If you need follow-up," he says, "the computer will do a dance in the doctor's office to make sure you get it."
Peddie feels the greatest opportunity for improving healthcare experience resides in empowering people to make educated choices for themselves. "Society has got to permit the industry to put a mission into the health delivery system," Peddie says.
Government Mandates Impact Affordability
C. Brooks Stone, vice president of product and program development at Blue Cross and Blue Shield of Florida (BCBSF), says that even in the business-to-business market, the individual still makes the ultimate choice among health plans. What individuals want, according to Stone, is choice. "Our members want us to offer a range of options - so they can determine what best meets their needs - and to keep their coverage affordable," he states.
BCBSF is the state's largest healthcare company, offering its over 2 million members a menu of traditional health insurance, PPO, point-of-service and HMO plans for small groups, large groups and individual buyers both over and under age 65.
Stone points out that many new and costly drugs result in more effective treatment of disease, but cost pressure in prescription drug claims also currently comes from lifestyle enhancement drugs and drugs that treat conditions not traditionally considered to be disease or health problems.
State and federal government mandates also create cost pressure in healthcare. These laws require all people buying health insurance to pay for coverage for specialized devices or procedures which benefit only a small portion of the population. At issue is affordability: Should the government require all healthcare consumers to purchase health benefits they do not not value?
Carriers used to control costs by limiting choice. But when members demand both choice and affordability, Stone says, the answer is to "open up the healthcare system and allow consumers to make informed choices."
BCBSF is preparing to do that in the near future, offering members real-time adjudication of claims, access to benefits descriptions, and the processing of approvals and referrals through computer links in providers' offices.. "I believe this will revolutionize the way people access healthcare," Stone concludes.
Early Intervention Saves Money
Most people want to be informed healthcare consumers. "Managed care brought this awareness to the equation," says Gene Roberts, executive director for Humana Workers' Compensation Services. When people are educated, he says, they make better decisions and the whole system is better off.
At Humana Workers' Comp, the necessary education begins with early intervention. "When someone's off work, we try to be an advocate and get them to the right providers quickly. We let them know it's our goal to get them back to work," Roberts explains. "To really manage medical costs, you must get people back to work."
In Florida, Humana Workers' Comp serves 350,000 people (about 5% of the workforce), including the managed care component of coverage for 160,000 State of Florida employees.
The strength of Humana Workers' Comp, Roberts says, is its Integrated Information Services, a systems solution to integrating the third-party-administrator and managed care operator functions. Historically, he explains, the two functions evolved separately, and the result has often been duplication of effort amid frustration and confusion for the injured, the doctors and the employers. Humana's team approach, Roberts says, lowers costs and results in smooth execution.
Getting Tough on Fraud
At Sarasota-based FCCI Insurance Group, a tough stance on fraud is part of the company's focus on saving policyholders money. FCCI's 45-person special investigations department and an in-house legal unit lead the crackdown against the estimated $100 billion a year insurance fraud problem in the U.S. The company implemented a toll-free fraud hotline, and anti-fraud flyers are inserted into every claims check.
FCCI's customers recognize additional savings thanks to the company's intensive loss control program. G.W. Jacobs, president and CEO, says the company maintains an average of three visits a year to insureds' operations. "That's two to three times greater than our competitors," he adds. "The result is better loss performance, which enables us to pay dividends of approximately 15% of premiums versus 6% for the industry average."
Founded in 1959, FCCI, has grown to become the country's 15th largest workers' compensation carrier. FCCI's product line has expanded to include other property and casualty lines as well as employee leasing products.
Providing Long-term Solutions
EBI Companies, part of Orion Capital Group and among the country's 20 largest workers' compensation providers, emphasizes client cost reduction and operational benefits through Zero Accident CultureR.
Todd Cicero, branch manager, Orlando, says the program's purpose is proactive loss prevention, through changing the workplace culture. "Often there's a contrast between management's perception that safety practices are in place and the worker's actual daily activities," Cicero says. EBI measures and quantifies change in the workplace culture over time, keeping management focused on impacting their losses and thereby keeping their premiums down. "We sell long-term cost solutions," Cicero says.
Claims management at EBI includes its Transitional Return to Work program, which addresses employee morale by treating every worker as part of the employer's success, and reduces clients' costs for lost time. In September, EBI will roll out a fully integrated on-line claims system. Cicero says this access will help customers see what's behind the scenes at EBI but that historically EBI's customers have been well satisfied working closely with their claims representative. "Our insureds are our partners," he says.
Retailers' SIF Stands Test of Time
Twenty years ago workers' compensation was often handled through self-insurers' funds. In Florida, most of these have converted into insurance companies or separated from their sponsoring organizations, but the oldest of them, Florida Retail Federation Self Insurers Fund, continues to serve the state's "Main Street" retailers. William B. Bull, president and CEO of Summit Consulting, FRF/SIF's administrator, says the Fund's 6,000 members receive very personalized service addressing their unique needs.
"Our typical client has seven or eight employees," Bull says, "and their workers' comp claims are very personal. Employers know the employee and they want him paid if he's entitled."
The Fund offers payment programs friendly to small business: the option to join with no down payment and to pay on a monthly basis on actual rather than estimated payroll. Bull says six of the original 10 members of FRF/SIF are still part of it, a testament to the continuing viability of the self-insuring concept in a changing world.
Summit Consulting, located in Lakeland, has administered SIFs and traditional insurance companies for 22 years.
Allowing the Insureds to Decide
Specialized service is just as critical to the risk management needs of multinational companies. Royal & SunAlliance, with offices in 132 countries, offers its larger accounts a risk-taking partnership in which RSA can cover crises ranging from ransom and extrication for kidnapped executives to the international transfer of blood or medicine. RSA's Management Assurancesm products include directors' and officers' liability, employment practices liability and fiduciary liability.
Business Development Manager John Warren, based at the firm's Tampa office, says management assurance products are a relatively new initiative for Royal & SunAlliance in the U.S. and Florida. RSA writes these policies flexibly to meet the needs of the client, offering high limits (up to $25 million per coverage part) and no "hammer clause" wherein an insured is pressed to settle a suit they'd like to litigate because the carrier will otherwise step out.
Warren says, "Executives don't want someone else to make the decision when it's their company's good name on the line." When RSA insureds elect not to settle, Warren explains, the company participates at a specified percentage up to the policy limit.
Relieving Benefit Frustrations
Small businesses can find customized support in healthcare solutions, workers' compensation and employee leasing through J. Rolfe Davis Insurance. From three offices in Orlando and Longwood, mobile service personnel and Internet access to claims information and benefits description, clients get a service level unusual among brokers.
David McKinney, president and CEO, says, "We try to get the best coverage for the best price for employer and employee, and then educate the employees on what they're getting." When workers don't understand their coverage and how to use it, McKinney explains, the intended employee benefit becomes a frustration instead.
Small businesses can shift the burden of administering benefits, McKinney says, to "employee leasing" or professional employer organizations (PEOs.) Through buying power and packaging, PEOs not only obtain healthcare coverage and workers' comp at wholesale prices, they can take over a range of "back room" functions including payroll. J. Rolfe Davis has formed its own PEO and will also broker the service.
Quantifying the Cost of Change
Aon Consulting provides integrated services in all forms of human resource management, including employee selection, benefit program design, change management and third-party administration of benefit plans. The Tampa office has a staff of 85 - including in-house actuaries, ERISA attorneys, investment advisors and a full print communications department - and a substantial systems commitment.
Richard Klima, senior vice president for health and welfare, says "disruption analysis" - capturing the effect of changing carriers - is an important Aon Consulting service. Clients can also conduct on-line file maintenance so that federally-mandated Summary Plan Descriptions are constantly updated and printable on demand. "Even some of our clients don't understand the breadth and depth of resources we bring to bear on these very complex issues," says Klima.
Klima points out that as cost pressures in the health and welfare marketplace increase, employers are likely to find themselves scrambling for savings on employee benefits plans. Aon Consulting is prepared to be very proactive in identifying problems in existing plans and enhancing the cost preventive aspects of plans, such as those that motivate employees toward healthier lives.
The Science of Business Efficiency
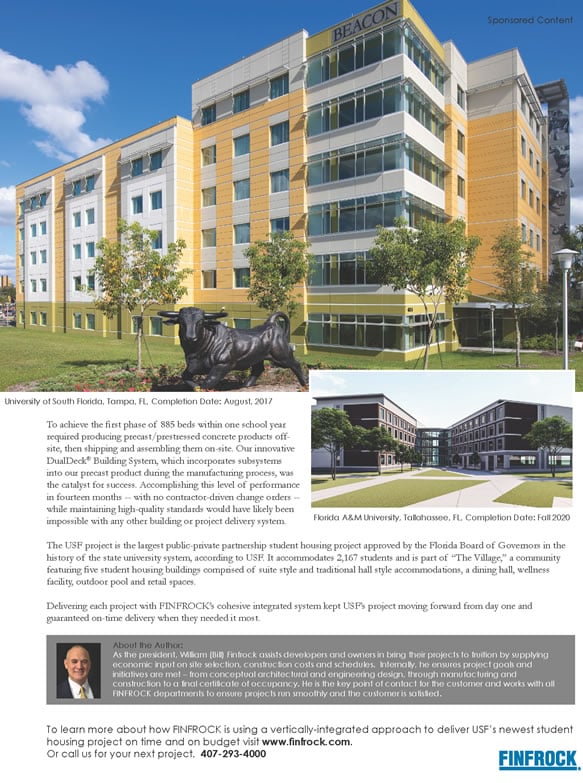
At H. Lee Moffitt Cancer Center & Research Institute at the University of South Florida in Tampa, the answer to excellent healthcare has been patience and good business sense. Dr. John Ruckdeschel, director, says that five years' effort at recruiting and mentoring good clinicians, plus paying careful attention to quality of patient care while running an academic center as a business has now paid off.
Moffitt has within the same year received a National Cancer Institute designation of excellence, one of only 60 centers around the country to do so, and "A" bond ratings by Moody's and S&P. "We take second to no one," Ruckdeschel says, "in science or business efficiency."
Florida Will Lead the Way
For Florida's medical practitioners, a key concern is the aging of the state's population. Harry K. Moon, M.D., CEO of Cleveland Clinic Florida, points out that in south Florida one in three people will be over age 65 in the year 2010. Noting that 95% of all healthcare expenditures are consumed in the final five years of a person's life, Moon is initiating roundtable discussions among the state's public and private sector healthcare leaders.
"Florida, along with California and Arizona, is going to lead the country in facing this issue," Moon says. "We need to generate a plan."
Cleveland Clinic Florida is a not-for-profit, multi-specialty group practice integrating community-based tertiary care with clinical and laboratory research and physician education. Patients from all over the region, the Caribbean and South America come to CCF to benefit from the care of a coordinated team of specialists. CCF also offers unique protocols and the creative energy of a teaching institution where, as Moon explains it, young physicians ask hard questions and drive everyone to look hard for answers.
To address a rising demand for services, CCF is expanding. In mid-2001, its Weston facility will become an integrated medical campus and its Naples site will add a hospital. Approval for open-heart surgery in Weston and kidney transplants in Broward has been granted by the Agency for Healthcare Administration.