Federal agents carry boxes of documents from Florida Home Health Care Providers in Miami in June. The operators were charged with filing $5.5 million in bogus claims. [Photo: Marice Cohn Band/Miami Herald] |
When George LeMieux, Florida’s new senator, was setting up house in Washington, D.C., recently, he went to Best Buy to pick up a television. Within minutes of his purchase, he says, he received a text message on his Blackberry from his credit card company asking him to confirm the purchase. Because LeMieux lives 700 miles away in Tallahassee, his credit card company’s computer systems had flagged the purchase as suspicious.
The experience inspired LeMieux to write his first bill. If credit card companies can use automated anti-fraud systems to protect consumers from theft, LeMieux reasons, then the federal government could use similar methods to combat healthcare fraud and corruption, a nationwide epidemic that is especially acute in south Florida. “Why can’t we set up the same model for the healthcare business so when a bad guy in Haines City sells the same wheelchair 100 times in the same hour, a flag goes off?”
The costs associated with healthcare fraud in the U.S. are staggering, between $68 billion and $226 billion a year.
Miami alone accounts for about $3 billion each year. In 2009, 227 people in south Florida were charged with Medicare fraud involving more than $951 million, according to the U.S. Department of Justice, and the region is widely recognized as the epicenter of healthcare fraud.
The schemes are varied but often involve clinic operators who submit bogus billings for HIV and cancer infusion therapies, purported home health agencies that submit claims for services never rendered, and fraudulent equipment suppliers who bill the government for canes, walkers, wheelchairs, oxygen equipment and artificial limbs that are never actually provided to patients.
|
||||||||||||||||||||||||||||||||
Some schemes involve licensed healthcare providers. In one case last year, for instance, Miami doctors Walter Proano and Manuel Barbeite billed Medicaid and Medicare for expensive medications intended to treat HIV/AIDS patients suffering from a rare illness. In fact, the doctors, who wrote prescriptions for large quantities of these medications, had little if any of the medications in stock and rarely, if ever, provided the infusions to their patients. All told, they and their associates defrauded Medicare and Medicaid out of nearly $16 million, according to government documents.
The scam business is also increasingly attracting organized crime figures and career criminals who are taking fraud to a new level.
When federal agents last June broke up a Miami fraud ring that had attempted to bilk Medicare and the Medicare Advantage program out of $100 million, even seasoned U.S. Attorney Jeffrey Sloman expressed surprise at the “sophistication and geographic breadth” of the conspiracy. According to indictments, Michel De Jesus Huarte and seven other Miami defendants allegedly used fake prescriptions, bribes and stolen Medicare information to submit fraudulent invoices for expensive cancer and HIV therapies. They fronted their scheme through six phony clinics in Miami-Dade County and other areas of the Southeast and laundered their profits through local check-cashing stores.
Joining the battle
While federal authorities have ramped up enforcement against such crimes in recent years, Florida lawmakers have also taken aim at the problem.
In 2007, lawmakers passed a bill mirroring the Federal False Claims Act that authorizes the state Attorney General’s Medicaid Fraud Control Unit to recover through a civil lawsuit three times the actual damages caused by those who commit Medicaid fraud. In 2008, the Legislature enacted strict licensing and reporting requirements for home healthcare agencies, which have been the source of a significant amount of Medicaid fraud.
In 2009, the Legislature approved a bill that targets home healthcare agencies with tougher Medicaid billing requirements and imposes harsher penalties for those who commit Medicaid fraud. The new regulations elevated Medicaid fraud from a third-degree felony to a first-, second- or third-degree felony based on the amount involved in the fraud. The bill also designated Miami-Dade County as a “healthcare fraud crisis area” for the purposes of increasing the monitoring of home health agencies, home medical equipment providers, clinics and other providers.
The law additionally prohibits the Agency for Health Care Administration from approving new home health agencies in Miami-Dade and Broward counties at least until July. The law also states that AHCA can revoke a home health agency’s license if it demonstrates a “pattern” of billing Medicaid for services that are later deemed unnecessary, with as few as two potential billings constituting a “pattern.”
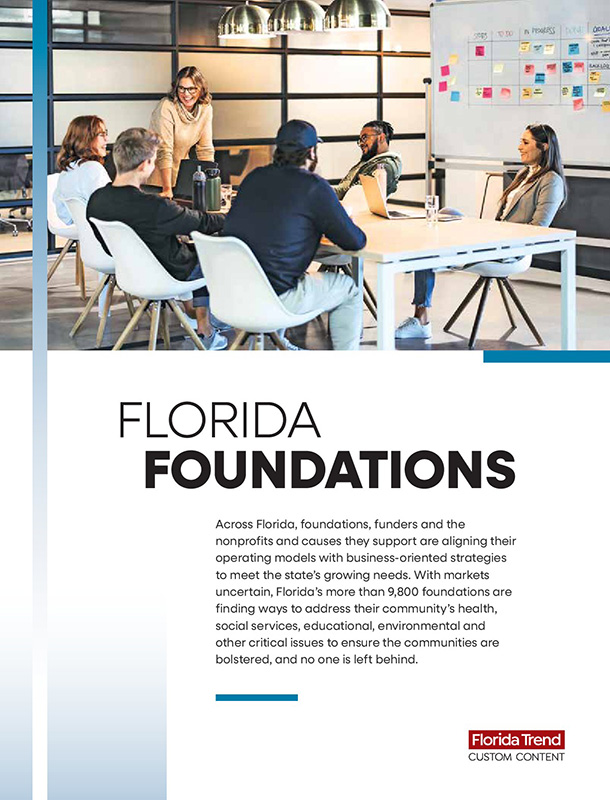
As Congress contemplates moves toward legislation that could dramatically expand the rolls of Medicaid, and increase potential for fraud, some believe that even more needs to be done.
Craig Smith, a Tallahassee lawyer and health law expert who previously served as general counsel for AHCA, says, “The fundamental change has to be in addressing prepayment prevention. This pay-and-chase system recovers such a small portion of the bad payments.”
Smith likes a pilot program the Florida Legislature passed in 2009 that would require Medicaid to verify telephonically the delivery of home health services using voice biometrics. The program, not yet started, would make committing fraud more difficult, says Smith.
In the book “Stop Paying the Crooks: Solutions to End the Fraud that Threatens Your Healthcare,” Smith says the federal government could do more to weed out cheats by improving the enrollment screening process for applications for new clinics, home health agencies and medical equipment suppliers. Smith also proposes that providers of “very expensive treatments and therapies” be required to meet enhanced prepayment review standards and that public and private payers could improve their information-sharing and coordination efforts to better crack down on fraud.